
Introduction
In the complex world of healthcare, patients often face hurdles when it comes to getting their prescribed medications covered by insurance. One of the most common barriers is prior authorization (PA). This process, used by health insurance companies and pharmacy benefit managers (PBMs), requires approval before certain prescription drugs or treatments are dispensed. While prior authorization is meant to ensure cost-effective and clinically appropriate care, it can delay treatment and create frustration for both patients and providers.
In this article, we’ll break down the prior authorization process for prescription drugs, explain why it exists, and provide insights into how patients and healthcare professionals can navigate it effectively.
What Is Prior Authorization in Prescription Drugs?
Prior authorization is a requirement from an insurance company or PBM that a healthcare provider must obtain approval before prescribing a specific drug. Without this approval, the medication may not be covered, and the patient could be responsible for paying the full cost out-of-pocket.
This process applies to medications that:
- They are high-cost or brand-only drugs.
- Have a generic alternative available.
- Pose safety risks or require strict monitoring.
- They are part of step therapy protocols, where patients must try lower-cost medicines first.
Why Do Insurance Companies Use Prior Authorization for Prescription Drugs?
The main reasons payers implement prior authorization include:
- Cost Control – Ensuring expensive medications are prescribed only when necessary.
- Clinical Appropriateness – Confirming that the drug is safe and effective for the patient’s condition.
- Formulary Compliance – Encouraging the use of drugs listed in the insurance plan’s formulary.
- Preventing Misuse – Reducing the risk of overprescribing controlled substances.
For insurers, PA is part of utilization management strategies that balance patient care with healthcare costs.
The Step-by-Step Prior Authorization Process for prescription drugs
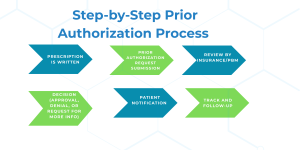
1. Prescription Is Written
A physician prescribes a medication. If that drug requires prior authorization, the pharmacy system flags it.
2. Prior Authorization Request Submission
The provider (or their staff) submits a PA request form to the insurance company. This form includes:
- Patient demographics.
- Clinical diagnosis.
- Previous treatments tried (step therapy evidence).
- Justification for why the drug is needed.
3. Review by Insurance/PBM
The insurance company’s medical or pharmacy team reviews the request. They check:
- Clinical guidelines.
- FDA approval status.
- Plan’s formulary restrictions.
4. Decision (Approval, Denial, or Request for More Info)
- Approval – The prescription is covered, and the patient can pick it up.
- Denial – The request is rejected, often citing alternatives.
- Pending/More Info Needed – Additional medical records are required.
5. Patient Notification
The provider and patient are notified of the outcome. If denied, the provider can appeal.
6. Track and Follow Up
Providers or staff should monitor the status of the PA request. Regular follow-up ensures timely approval and helps address any additional information requests promptly.
Common Challenges in the Prior Authorization Process
1. Delays in Treatment
The process can take days or weeks, leading to frustration and potentially worsening conditions. You can also check how long does prior authorization take for medication.
2. Administrative Burden
Providers and staff spend significant time filling out PA forms, making calls, and appealing denials.
3. Patient Confusion
Patients may not understand why their prescribed drug isn’t immediately available.
4. Denials and Appeals
Denials are common, and appeals require strong clinical documentation.
How Long Does Prior Authorization Take?
The timeline varies by insurer and medication:
- Electronic prior authorization (ePA): 24–72 hours.
- Manual fax or phone requests: 5–10 business days.
- Urgent requests: May be reviewed within 24 hours.
Despite technology, many providers still face bottlenecks due to incomplete forms or insurer backlogs.
Tips for Patients Navigating Prior Authorization
- Ask Upfront – When prescribed a new drug, ask if prior authorization is required.
- Stay Informed – Understand your insurance formulary and covered drug list.
- Communicate with Your Doctor – Ensure the provider submits all necessary documentation.
- Explore Alternatives – If denied, ask about generics or formulary-preferred drugs.
- File an Appeal – Patients have the right to appeal insurance denials.
How Providers Can Streamline the PA Process
- Use Electronic Prior Authorization Tools – Many EHR systems now integrate ePA systems for faster processing.
- Assign PA Specialists – Larger practices employ staff dedicated to handling PA requests.
- Submit Complete Documentation – Missing details cause delays.
- Track Requests – Follow up regularly to avoid unnecessary waiting.
- Educate Patients – Helping patients understand the process reduces frustration.
The Future of Prior Authorization
The healthcare industry is moving toward more automation and standardization in PA processes. Key trends include:
- Electronic prior authorization (ePA) adoption across pharmacies.
- AI-driven utilization management to reduce manual work.
- Legislative reforms in the U.S. are pushing for faster decisions and patient protections.
- Value-based care models are reducing unnecessary PAs by aligning payment with outcomes.
.
Conclusion
The prior authorization process for prescription drugs is a crucial part of healthcare utilization management, designed to ensure safe, cost-effective, and clinically appropriate treatment. However, it often creates challenges for patients and providers, including delays, administrative workload, and denial disputes.
By understanding the process, staying proactive, and using electronic tools, both patients and healthcare providers can navigate prior authorization more effectively. The future promises more streamlined, automated systems that prioritize patient access without compromising quality or cost efficiency.
FAQs
1. What is the prior authorization process for prescription drugs?
The prior authorization process for prescription drugs is when your doctor must get approval from your insurance provider before a specific medication is covered. This ensures the drug meets the plan’s medical necessity and formulary requirements.
2. What are the key PA steps involved?
The main PA steps include: prescription written, request submission, insurer review, approval or denial, and patient notification. Delays usually happen if documentation is incomplete.
3. Which medications usually require prior authorization?
Drugs that are expensive, brand-only, high-risk, or part of step therapy protocols often need prior authorization. These drug authorization requirements help insurers manage safety and costs.
4. How long does the prior authorization process take?
Electronic prior authorization (ePA) usually takes 24–72 hours, while manual requests may take 5–10 business days. Urgent requests can sometimes be processed within 24 hours.
5. Can a prior authorization request be denied?
Yes. Denials may happen if documentation is incomplete, the drug is not on the formulary, or the insurer prefers a lower-cost alternative. In such cases, providers can appeal with stronger clinical justification.
6. How can patients speed up the prior authorization process?
Patients can ask upfront if prior authorization is required, ensure their provider submits complete documentation, and request expedited review if the situation is urgent.
7. How are providers reducing prior authorization delays?
Many providers now use electronic PA tools, assign staff to handle prior authorizations, and educate patients about drug authorization requirements to avoid confusion and delays.


